
(Photo by Pavel Danilyuk)
As life expectancy increases and our lifestyle and diet change, humanity faces increasingly complex conditions and diseases. Modern medicine is more and more capable of dealing with quite a few of them under one important condition: early diagnosis.
Dementia (from Latin — “without mind”) is a neurological disease characterized by a deterioration in mental abilities, impaired concentration, etc. It is usually a “disease of old age” and one (but not the only one) of its types is Alzheimer’s disease.
Some of the early indicators of dementia can appear a decade before the onset, and if the closest people recognize them, can “sound an alarm” so that timely action can be taken against it. My personal experience with my father and my aunt, in various stages of cognitive decline, motivated me to closer study this topic.
One such sign is a decline in coordination, affecting the ability to control movement. This may manifest as difficulty catching objects, such as those being thrown or dropped, or as reduced precision and control when using tools or utensils.
Additionally, there may be an increase in clumsiness, characterized by tripping, stubbing toes, or bumping into objects while moving. Fine motor skills, such as shaving, combing hair, buttoning shirts, tying shoelaces, or ties, may also become challenging. Mild tremors, characterized by slight shaking of the hands, may also occur.
These symptoms collectively indicate a decrease in motor control. It is important to note that these signs do not necessarily indicate the progression to dementia. However, they suggest that brain cells are not functioning as optimally as they once did, and over time, degeneration of the brain can increase the likelihood of developing dementia.
A crucial understanding of dementia and other disease processes is that our current standard model is flawed. Traditionally, we perceive disease as occurring abruptly, with a period of healthy living followed by a sudden onset of symptoms. However, this model does not accurately reflect the reality of many diseases.
In the case of dementia, for instance, symptoms may not appear until later in life, around the age of 50. Individuals may visit the doctor due to general discomfort or other health concerns, only to receive a diagnosis of dementia. This diagnosis can be perceived as a sudden onset of illness, disregarding the gradual progression of symptoms over time.
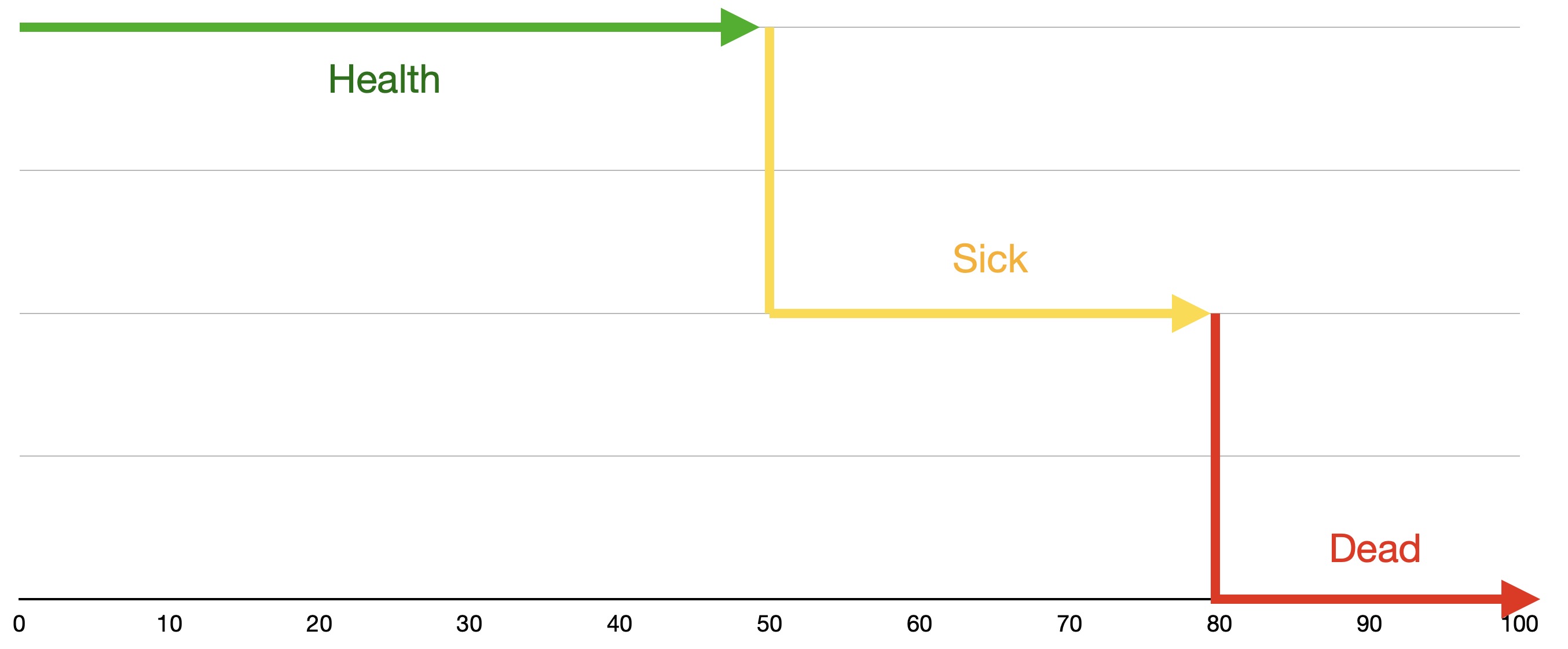
The conventional approach to managing this condition involves treating symptoms with medication. However, this approach does not address the underlying causes and may not yield significant improvements in overall well-being. Over time, individuals typically reach the age of 80 or slightly older, when they experience a rapid decline in health, often resulting in premature death. This progression is not a sudden, black-and-white event but rather a gradual functional decline.
In reality, individuals possess a certain level of function that gradually decreases over time. Initially, this function may be at 100%, but as individuals age, their bodies undergo a natural process of development and degeneration. This process is conditioned and programmed to occur, resulting in a gradual decline in function. At the age of 20 or slightly older, individuals typically reach their peak functional capacity. However, this capacity gradually declines over the years, with each year bringing a loss of a few percent of function.
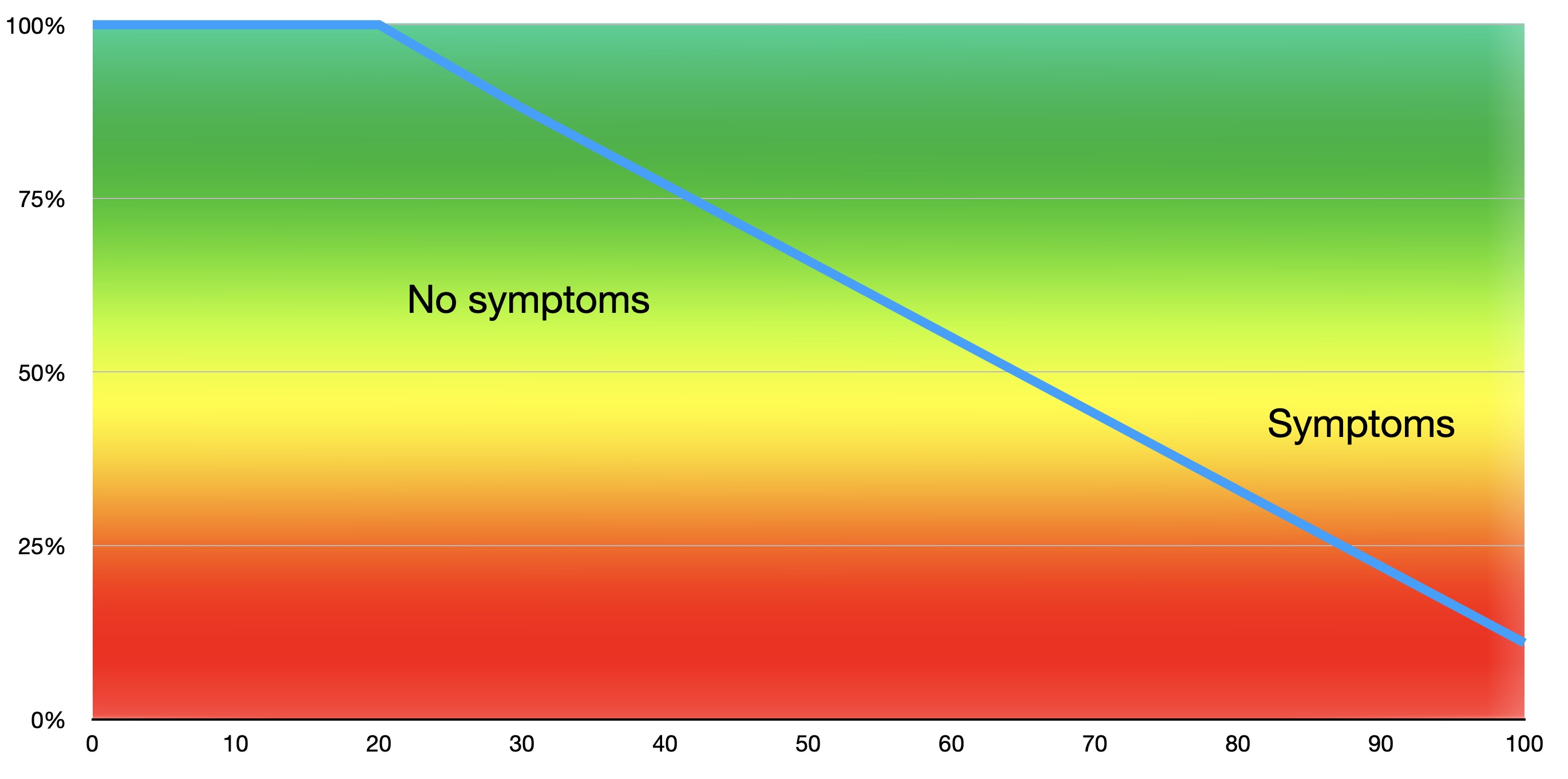
While this decline may not be immediately noticeable and may not cause symptoms, it eventually reaches a point where individuals begin to experience noticeable symptoms. It is important to note that this progression is not a sudden event but rather a gradual development that may appear abrupt.
Adhering to the standard model of treatment, which primarily focuses on symptom management with medication, does not address the root causes of the condition. This approach does not provide additional support or resources for the body’s functioning, leading to a continued decline in function until the point of complete loss. Understanding the functional model, which emphasizes the decline in energy levels after the age of 20, prompts the question of when to take proactive steps to address this decline. Every bodily function is essential, and there are no spare parts or optional components. However, it is argued that the brain holds the most significance as it controls and regulates all other bodily functions. The brain is the foundation upon which all other aspects of health and well-being depend.
Therefore, addressing the decline in brain function is crucial for maintaining overall health and quality of life. In essence, the brain holds paramount importance for the overall quality of life. There exists a direct correlation between the health of the brain and the quality of life. Notably, the brain is one of the organs that presents the greatest challenge in terms of regeneration. While it does not imply that regeneration is entirely impossible or that it invariably declines linearly, it is undoubtedly more arduous compared to other organs.
One of the primary reasons for this difficulty lies in the presence of a point of no return. This occurs when cognitive function and brain activity deteriorate to a certain extent, rendering it virtually impossible to reverse the decline. Consequently, the brain relies solely on itself to initiate and sustain a positive trajectory. In contrast, the heart can be restored to a healthier state through appropriate nutrition and other interventions, but the brain demands the same level of commitment and motivation to maintain and enhance its quality of life and facilitate regeneration.
Therefore, it is imperative that we recognize the significance of the brain as the most crucial organ, regardless of our age or level of cognitive function. By promptly understanding its intricacies and identifying its specific needs, we can effectively enhance and sustain its function for an extended period.
As a nutrition coach, I would like to address the concerns of parents regarding their children’s health. While it is reassuring to know that your children are not currently afflicted with dementia, it is essential to recognize that the risk of developing cognitive decline increases with age. Consequently, it is crucial to take proactive steps to maintain and enhance your children’s brain health. One common challenge faced by parents is the presence of junk food in their homes. While it may be tempting to believe that you can maintain a healthy diet for a week, the constant availability of junk food for your children can pose significant obstacles to your efforts. It is important to consider the impact of junk food on your children’s health and well-being. Why would you want your children to consume unhealthy food and end up in the same predicament as you, with a diagnosis? Why not educate them at an early age about proper nutrition and bodily functions to prevent them from developing similar issues?
The next indicator is related to gait, posture, and movement. It could be as simple as a shuffling gait, characterized by dragging the feet or shorter steps, a reduced stride length, or a loss of spring in the step. Alternatively, it could manifest as a stooped or hunched posture. How many individuals do you observe developing these symptoms as they age? Even subtle changes can be significant indicators.
One of the most prevalent signs is anterior head carriage, but it can also be internal rotation. If you notice people’s arms hanging straight down parallel to their bodies, but they turn inward slightly, it suggests a diminished ability of the brain to suppress the muscles responsible for hand rotation. Internal rotation is a sign of stress and brain degeneration. It can also be associated with anterior head carriage, shoulder internal rotation, and shoulder elevation, all of which are manifestations of the same underlying mechanism. If you pay attention, you will also observe hip and knee flexion as part of this pattern involving internal rotation. When the head moves forward, the hands turn inward, and simultaneously, the hips move backward slightly, and the knees bend.
The stronger the brain, the stronger its ability to maintain this posture. Conversely, as the brain weakens, we observe a gradual progression of these signs to varying degrees. In the realm of neuroscience and neurology, it is crucial to recognize that all observable symptoms and diagnostic indicators serve as therapeutic interventions. This principle implies that if an individual observes a particular condition, such as anterior head carriage, and actively works on improving their posture, shoulder alignment, and overall gait, they are actively constructing the neural pathways that support these functions. The concept of “use it or lose it” applies here, as consistent attention and practice enhance the brain’s ability to maintain these functions.
Furthermore, individuals may notice a distinguishable stiffness in their gait and movements, resulting in a decrease in smoothness and fluidity. Additionally, there may be alterations in balance and spatial awareness, the ability to perceive and respond to the environment without conscious attention. As these abilities decline, individuals may experience unsteadiness while standing or walking. This could manifest as stumbling, either directly or as a perceived stumbling sensation that necessitates grasping or holding onto objects.

(Photo by Mikhail Nilov)
Misjudgments in distance and timing, particularly regarding stationary and moving objects, may also occur. Furthermore, multitasking while moving becomes more challenging, requiring individuals to prioritize tasks, such as walking and turning simultaneously, rather than simultaneously performing both actions. Regarding muscle and body movement, you may notice a simple yet significant change: muscle stiffness, where your body’s stretching and relaxation abilities diminish. This is particularly evident in spinal stiffness, which underscores the crucial role of yoga, tai chi, and qigong in maintaining spinal flexibility.
The importance of this is because approximately 90% of the signals that sustain brain function originate from the body, including movement and gravity. The spine houses a vast majority of these signals, with a higher concentration of receptors for movement and spatial awareness, known as proprioception (from Latin: proprius – own, peculiar, receptor – receiving and capio, cepi – to receive, to perceive; in English: proprioception; also called kinesthesia from Ancient Greek: κοινός - common + αἴσθησῐς – feeling, sensation; in French: cénesthésie): the muscular sensation and sense of self-movement and position of one's body parts, relative to each other, and in space, sometimes described as a "sixth sense". As the brain ages and declines due to a lack of these signals, spinal stiffness ensues. However, maintaining spinal flexibility allows these signals to flow, preserving brain function.
Another potential issue is restless legs syndrome. While it is understandable to associate restless legs with dementia, it is important to note that this can be a symptom of brain decline. However, there are other contributing factors, such as inflammation, pH levels, and mineral status.
Finally, we address the most common concern: mild cognitive decline. This manifests as forgetfulness of names, words, tasks, or even recent events. While it is normal to experience occasional forgetfulness, it becomes a concern when it becomes frequent or severe. Mild cognitive decline can also lead to difficulty concentrating and organizing. As cognitive decline progresses, maintaining focus on a single task and effectively managing multiple tasks becomes increasingly challenging. This can lead to difficulties in completing complex tasks that require sustained, focused attention. Additionally, individuals may experience mind-wandering, making it challenging to stay on task. However, mind-wandering can also be triggered by engaging in conversations, potentially affecting communication skills. Some subtle changes in speech patterns may occur, such as slower speech or occasional slurring, which can be challenging to pronounce or form correctly. Finding words can also become difficult, a common experience that varies in frequency and severity.
Other physical manifestations of cognitive decline include reduced facial expression. Facial muscles exhibit less movement, resulting in less animated speech and a diminished emotional impact. Emotional expression in speech involves the use of intonation, variation, and the overall melody of the words. A lack of emotional expression can make speech sound flat and monotonous, akin to droning.
The slowing of the brain can also impact handwriting. One way handwriting can be affected is through micrographia, a condition characterized by progressively smaller handwriting as control becomes increasingly difficult. This can manifest as sloppy and illegible handwriting, deviating significantly from the neat and organized style of the past. With digital communications nowadays (text messages, emails, etc.), frequent misspellings or lexical errors (due to the random use of autocorrect) can express the same process.
Another potential outcome is that people become more irritable. They may experience outbursts or simply feel more irritable in general. This is because one of the primary functions of the brain is to suppress and regulate emotions. As an irritation arises or an outburst approaches, a well-functioning brain can dampen it and provide perspective. However, when the brain’s function weakens and slows, it may struggle to control these outbursts or emotions effectively.
Social withdrawal can also occur, where individuals withdraw from their communities due to the energy required or because the experience no longer provides the same level of reward. Anxiety and depression can also manifest, as the brain’s primary function is to suppress these negative thoughts. Consequently, a healthier brain facilitates an easier elevation of mood.
Empathy can also be impaired, making it challenging to understand and interpret others’ emotions and motivations. This can lead to difficulty in comprehending others’ actions and a diminished emotional connection. Fatigue can also develop, even after sufficient sleep. Additionally, fatigue may occur after minimal exertion, which is unusual and should not cause tiredness. Sleep disturbances can also occur, as proper and restful sleep is closely linked to a well-functioning brain. Frequent napping may also be necessary.
Movement has high importance, and it is evident that many of the symptoms mentioned relate to movement. Furthermore, I have already explained that 90% of the brain’s input is related to movement. The primary purpose of the brain is to process information. In essence, the majority of the input the brain receives from movement sustains its vitality. The close connection between brain function and movement explains why subtle signs related to movement are often detected early. However, it is crucial to recognize that movement is not the sole factor influencing dementia. Other aspects, such as genetics and inflammation, also play significant roles.
While these subtle signs provide valuable insights, they do not guarantee a direct 100% association between movement and dementia. Nevertheless, it is essential to understand that all these signs indicate brain degeneration. As the brain degenerates, brain function declines, increasing the likelihood of developing dementia. These early signs suggest a lesser quality of neural network degeneration, reduced energy production, and impaired cellular energy production. Consequently, the brain’s ability to control movement and function diminishes, leading to a reduced capacity for rapid and efficient processing.
To combat this degeneration and improve overall well-being, adopting a holistic approach is vital. Three key components are essential:
1. Nutrition
Eating a balanced diet is crucial to avoid low-grade inflammation, metabolic syndrome, and toxicity. Learn how to make informed food choices and maintain a healthy diet.
2. Physical Activity
The body is inherently designed for movement. Regular exercise, such as taking 10,000 steps and incorporating stretching, can significantly contribute to overall health. While daily gym sessions may not be necessary, incorporating movement into daily life is beneficial.
3. Cognitive Enhancement
Practicing better thinking habits can lead to improved mood and overall well-being. Reading positive content, engaging in relaxation exercises, practicing breathing techniques, and incorporating meditation into daily routines can enhance cognitive function and reduce stress.
In essence, maintaining a positive outlook, practicing cognitive enhancement, and adopting a healthy lifestyle are essential components of achieving optimal health and preventing dementia. Additionally, sensory changes can occur, with anosmia being one of the most prevalent. This condition can lead to the inability to recognize certain objects or alter the perception of familiar scents, such as coffee or food. A subtle sign of sensory loss may also involve difficulty interpreting sounds, particularly in noisy environments. This is not a reflection of a lack of sensory apparatus but rather the complex process of interpreting and creating a three-dimensional image of sound in the brain. Even with normal hearing, the brain’s ability to function can be affected, potentially impacting sound interpretation.

(Photo by cottonbro studio)
Vision can also be affected, with reduced distance judgment based on visual cues, light perception, and neural impulse generation. This process is further complicated by the brain’s role in creating a visual representation. Furthermore, dim light can impair movement and object recognition, and decision-making processes may become slower and more indecisive.
These subtle changes can also affect executive function, leading to outbursts of impulsive behavior. If the brain’s ability to control impulses is compromised, spontaneous outbursts may become more frequent. These outbursts could indicate poor choices, potential safety risks, or financial mismanagement, such as overspending due to a lack of appropriate limits. Decision-making may become more challenging, with hesitation and indecisiveness replacing clarity and ease. Spontaneity may decrease as motivation wanes, and activities that once brought joy now seem unappealing. Financial management may become overwhelming, with complex tasks like tracking bills and paying them on time becoming daunting.
It is crucial to recognize that the brain controls every aspect of our lives, and everything happens for a reason. Even seemingly random movements, such as arm swings, have underlying meanings and serve a purpose. While it is not necessary to assume that every aspect of life must be of utmost importance, it is crucial to recognize that even seemingly insignificant matters are directly influenced by the functioning of the brain. By paying attention to these small details and making gradual improvements, we can collectively enhance the overall efficiency of our cognitive abilities.
